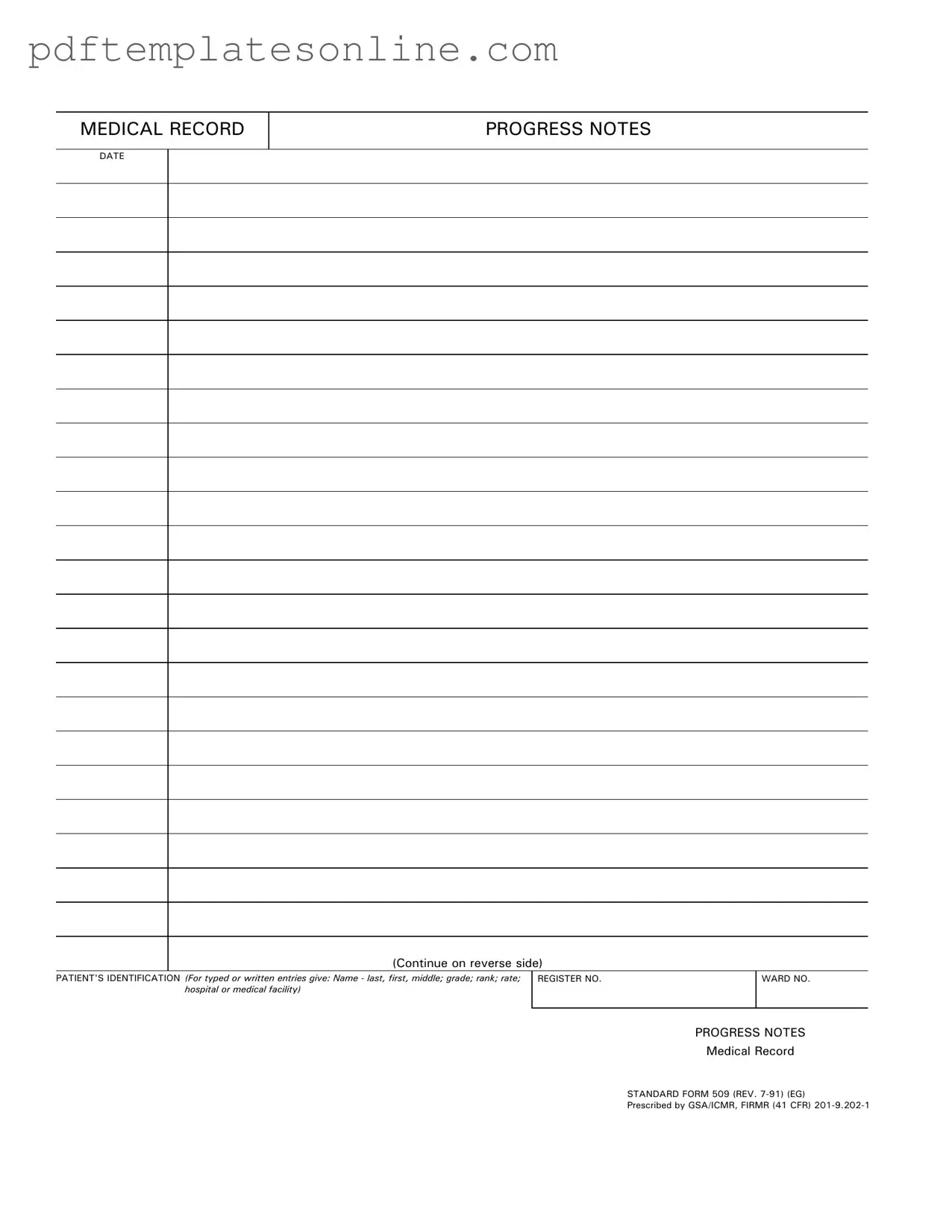
Blank Progress Notes Form
Key takeaways
When it comes to filling out and utilizing the Progress Notes form, understanding its components and purpose is crucial. Here are some key takeaways to consider:
- Accurate Patient Identification: Always include the patient's full name, grade, rank, and rate. This information is essential for proper record-keeping and patient identification.
- Register and Ward Numbers: Make sure to fill in the register number and ward number. These identifiers help in organizing and locating patient records efficiently.
- Date of Entry: Record the date on which the notes are made. This provides a timeline of the patient's care and treatment.
- Clear and Concise Notes: Write progress notes in a clear and straightforward manner. This ensures that anyone reviewing the notes can quickly understand the patient's status and treatment plan.
- Confidentiality is Key: Always handle the Progress Notes form with care. Protect patient information to maintain confidentiality and comply with privacy laws.
- Use of Standard Form: Familiarize yourself with the Standard Form 509. It is designed to streamline the documentation process and ensure consistency across medical records.
- Review and Update: Regularly review and update progress notes as necessary. Keeping records current is vital for effective patient care and communication among healthcare providers.
Common mistakes
Filling out the Progress Notes form accurately is crucial for maintaining clear and effective medical records. However, several common mistakes can lead to confusion and potential issues down the line. Understanding these pitfalls can help ensure that the form is completed correctly.
One frequent error is failing to include all necessary patient identification details. Each entry should contain the patient's full name, including last, first, and middle names. Omitting this information can create difficulties in tracking patient history and treatment. Always double-check that the identification section is fully completed.
Another mistake often made is neglecting to update the date of the entry. Each Progress Note should reflect the date it was completed. Without this critical information, it becomes challenging to maintain a chronological record of patient care. Ensure that the date is clearly written and corresponds to the day the notes were made.
In addition, many individuals overlook the importance of using the correct format for the medical record number and ward number. These identifiers are essential for proper organization and retrieval of patient records. Using an incorrect or incomplete number can lead to significant delays in accessing patient information. Always verify these numbers before submission.
Additionally, some entries may lack sufficient detail in the Progress Notes section itself. It’s vital to provide a clear and concise account of the patient’s condition, treatment, and any changes observed. Vague notes can lead to misunderstandings among healthcare providers. Take the time to articulate observations accurately.
Lastly, a common oversight is failing to sign or initial the form. Each Progress Note must be authenticated by the individual completing it. This step confirms accountability and ensures that the information can be traced back to the responsible party. Always remember to sign the document before submitting it.
Misconceptions
Misconceptions about the Progress Notes form can lead to confusion and mismanagement of patient records. Here are ten common misconceptions, along with clarifications for each.
- Progress Notes are only for doctors. Many believe only physicians can fill out Progress Notes. In reality, various healthcare professionals, including nurses and therapists, can document their observations and treatments.
- Progress Notes must be lengthy. Some think that detailed entries are always necessary. However, concise and clear notes that capture essential information are often more effective.
- All entries in Progress Notes are confidential. While Progress Notes are generally protected, there are circumstances where they can be disclosed, such as during legal proceedings or with patient consent.
- Progress Notes are optional. This is a significant misconception. Progress Notes are a critical component of patient care and must be completed to ensure continuity and quality of treatment.
- Progress Notes can be written in any format. There is a standard format for Progress Notes that must be followed to maintain consistency and clarity across medical records.
- Corrections in Progress Notes are not allowed. While it is important to avoid errors, corrections can be made. However, they should be documented properly to maintain the integrity of the record.
- Progress Notes are only for inpatient care. Many think these notes are limited to hospital settings. In fact, Progress Notes are used in various healthcare environments, including outpatient clinics and home health care.
- Progress Notes are not reviewed by others. Some assume that only the person who writes the notes will read them. In reality, they are often reviewed by other healthcare providers involved in the patient's care.
- Progress Notes are only for tracking medical issues. While they do track health concerns, Progress Notes also document patient progress, treatment plans, and responses to therapies.
- Progress Notes do not require signatures. This is incorrect. Most Progress Notes must be signed by the healthcare provider to verify the authenticity and accountability of the information documented.
Dos and Don'ts
When filling out the Progress Notes form, it's essential to follow certain guidelines to ensure accuracy and clarity. Here’s a list of what to do and what to avoid:
- Do include the patient's full name, including last, first, and middle names.
- Do provide the patient's grade, rank, or rate as applicable.
- Do ensure the registration number and ward number are filled out correctly.
- Do write legibly, whether you are typing or handwriting the entries.
- Don't leave any sections blank; fill out all required fields.
- Don't use abbreviations that could lead to confusion or misinterpretation.
- Don't forget to date each entry accurately.
- Don't use white-out or any correction fluid; instead, cross out mistakes neatly.
By adhering to these guidelines, you can help ensure that the Progress Notes are clear, comprehensive, and useful for all healthcare providers involved in patient care.
Other PDF Forms
Nc4p - Changes in personal circumstances, like losing head of household status, affect when a new NC-4 must be filed.
In order to facilitate a smooth transaction, having access to templates such as the California PDF Forms can be extremely beneficial for both buyers and sellers looking to navigate the complexities of the real estate market in California.
Florida State Return - Whether you are an individual or a business, the Tax POA DR 835 is a versatile tool for managing tax issues effectively.
Detailed Guide for Writing Progress Notes
Completing the Progress Notes form is an important step in maintaining accurate medical records. After gathering the necessary information, you will be ready to fill out the form systematically. Follow these steps to ensure that all required details are included and correctly documented.
- Start by entering the date at the top of the form. This is essential for tracking the timeline of patient care.
- In the PATIENT'S IDENTIFICATION section, provide the patient's name. Include the last name, first name, and middle initial if applicable.
- Next, indicate the patient's grade, rank, or rate, depending on their status. This information helps categorize the patient appropriately.
- Identify the hospital or medical facility where the patient is receiving care. This ensures that the notes are linked to the correct location.
- Fill in the REGISTER NO. and WARD NO. as required. These numbers help in organizing patient records efficiently.
- Finally, in the PROGRESS NOTES section, write down the relevant observations, treatments, and any changes in the patient’s condition. Be clear and concise.
Once the form is completed, it will serve as a vital record of the patient's progress and care. Ensure that all entries are accurate and legible before submitting the form to the appropriate medical record department.