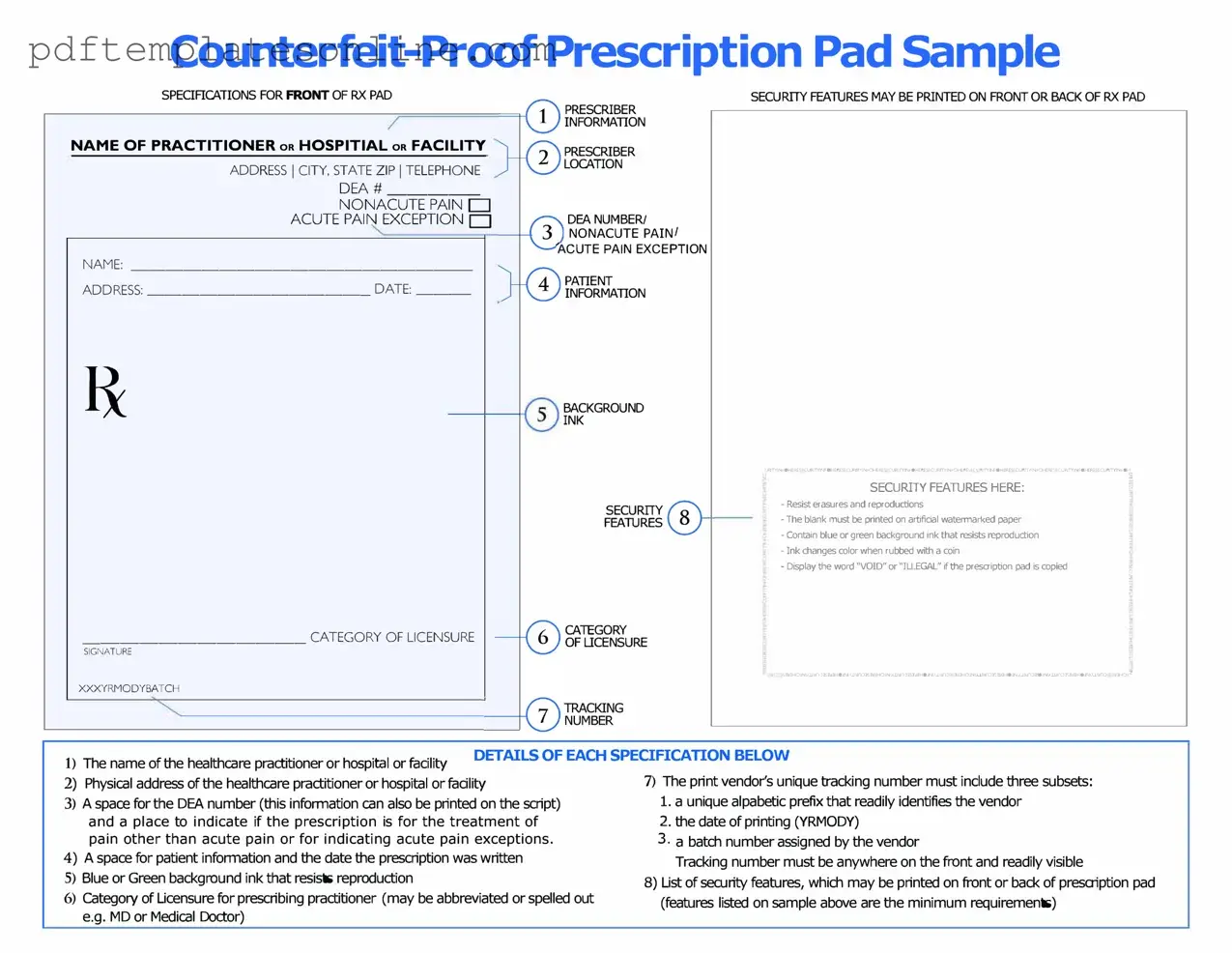
Blank Prescription Pad Form
Key takeaways
When using the Prescription Pad form, keep these key points in mind:
- Accuracy is crucial. Ensure that all information is filled out correctly to avoid any issues with medication fulfillment.
- Complete all sections. Each part of the form must be filled out, including patient details and medication information.
- Use clear handwriting. If you are filling out the form by hand, make sure your writing is legible to prevent misunderstandings.
- Specify dosage and instructions. Clearly state how much medication the patient should take and how often.
- Include your contact information. Provide your phone number or email in case the pharmacy needs to reach you for clarification.
- Sign and date the form. Your signature is necessary to validate the prescription, and dating it helps track when it was issued.
- Keep a copy for your records. Retaining a copy can be helpful for future reference and tracking patient care.
- Stay updated on regulations. Be aware of any changes in prescription laws or guidelines that may affect how you fill out the form.
Common mistakes
Filling out a Prescription Pad form can seem straightforward, but many people make common mistakes that can lead to delays or complications in receiving their medications. One frequent error is not providing complete patient information. Missing details like the patient's full name, date of birth, or address can cause confusion and may result in the pharmacy being unable to process the prescription.
Another common mistake is failing to specify the medication dosage clearly. If the dosage is unclear or ambiguous, the pharmacist may interpret it incorrectly, which could lead to serious health risks. It's essential to write the dosage in a clear and legible manner, ensuring that it is easily understood.
People often overlook the importance of including the quantity of medication prescribed. Omitting this information can lead to the patient receiving either too little or too much of their medication, which can affect their treatment plan. Always double-check that the quantity is clearly stated.
Additionally, many individuals forget to include the prescribing physician's signature. Without this crucial step, the prescription is not valid. It is vital to ensure that the signature is present and that it matches the name printed on the form.
Another mistake is not providing clear instructions for the pharmacy. For instance, if there are specific directions for how the medication should be dispensed or if there are any special considerations, these should be noted clearly. Lack of instructions can lead to confusion and delays in medication availability.
Some people also make the mistake of using abbreviations or shorthand that may not be universally understood. While it might seem convenient, using clear and complete language helps avoid misunderstandings that could jeopardize patient safety.
It’s also important to check for any allergies or interactions with other medications. Neglecting to include this information can put the patient at risk. Always ensure that any known allergies are clearly noted on the form.
Another common oversight is failing to update the Prescription Pad form for refills. If a patient requires refills but this is not indicated on the form, they may find themselves without necessary medication when they need it most. Clearly marking the number of refills can save time and hassle later on.
Lastly, some individuals may not check the expiration date of the Prescription Pad form itself. Using an expired form can result in the pharmacy refusing to fill the prescription. Always verify that the form is current before submission.
By avoiding these common mistakes, individuals can ensure a smoother experience when filling out the Prescription Pad form. Taking the time to double-check each section can lead to better health outcomes and a more efficient process for obtaining medications.
Misconceptions
Understanding the Prescription Pad form can be challenging, and several misconceptions often arise. Here are seven common misunderstandings about this important document:
-
Prescription Pad forms are only for controlled substances.
This is not true. While Prescription Pad forms are commonly associated with controlled substances, they can also be used for non-controlled medications. It is essential to understand that the form serves as a means to communicate medication instructions, regardless of the drug's classification.
-
Any healthcare provider can use a Prescription Pad form.
Not every healthcare provider has the authority to issue prescriptions. Only licensed professionals, such as physicians, nurse practitioners, and physician assistants, can legally complete and sign a Prescription Pad form.
-
Once a Prescription Pad form is signed, it cannot be changed.
This is a misconception. If a healthcare provider needs to modify a prescription after it has been signed, they can do so by issuing a new form or by making clear annotations on the original, as long as it complies with state regulations.
-
Prescription Pad forms are the same in every state.
This is incorrect. Each state has its own regulations regarding Prescription Pad forms, including what information must be included and how they should be formatted. Familiarity with local laws is crucial for compliance.
-
Patients can fill out the Prescription Pad form themselves.
Patients should not fill out the Prescription Pad form. This document must be completed by a licensed healthcare provider to ensure that the prescription is valid and safe for the patient.
-
All prescriptions require a physical Prescription Pad form.
In many cases, electronic prescriptions are valid and increasingly common. Many states allow healthcare providers to send prescriptions electronically, which can streamline the process and enhance security.
-
Prescription Pad forms are only necessary for new medications.
This is misleading. Prescription Pad forms can also be used for refills or adjustments to ongoing medication regimens. Healthcare providers may issue a new form to authorize a refill or change dosage, ensuring proper documentation.
By clarifying these misconceptions, individuals can better understand the role and function of the Prescription Pad form in the healthcare system.
Dos and Don'ts
When filling out the Prescription Pad form, it's important to ensure accuracy and clarity. Here’s a list of things you should and shouldn’t do:
- Do double-check the patient’s name and date of birth to avoid any mix-ups.
- Do write legibly to ensure that the pharmacist can read the prescription without confusion.
- Do include the dosage and frequency of the medication clearly.
- Do sign and date the prescription to validate it.
- Don't use abbreviations that may not be universally understood.
- Don't forget to include any special instructions for the patient.
Following these guidelines will help ensure that the prescription is filled correctly and efficiently.
Other PDF Forms
What Is Make Ready - Landlords can proactively address any cosmetic issues to enhance appeal.
A California Real Estate Purchase Agreement form is a crucial document used in the process of buying or selling real estate in California. It outlines the terms and conditions of the sale, including the purchase price, financing details, and inspection rights. This legal document ensures that both parties, the buyer and the seller, understand their rights and obligations. For those seeking additional resources, California PDF Forms can provide helpful templates and guidelines.
Work Application Form - Provide your LinkedIn profile if requested for additional professional insight.
Detailed Guide for Writing Prescription Pad
Completing the Prescription Pad form is straightforward and ensures that all necessary information is captured accurately. Follow these steps carefully to fill out the form correctly.
- Start by writing the patient's full name at the top of the form.
- Next, enter the patient's date of birth. Use the format MM/DD/YYYY.
- Provide the patient's address, including street, city, state, and zip code.
- Write the date of the prescription in the designated area.
- List the medication name clearly. Include the dosage and frequency of use.
- Indicate the quantity of medication to be dispensed.
- Sign the form with your name and credentials.
- Finally, add any additional instructions for the pharmacist if necessary.
After completing these steps, the form is ready for submission to the pharmacy. Ensure that all information is legible and accurate to avoid any delays in processing the prescription.