Official Pennsylvania Do Not Resuscitate Order Document
Key takeaways
When filling out and using the Pennsylvania Do Not Resuscitate Order (DNR) form, it is essential to consider the following key takeaways:
- Eligibility: The DNR order is intended for individuals who have a serious illness or are nearing the end of life. It is crucial to assess the medical condition of the person for whom the DNR is being completed.
- Completion Process: The form must be completed and signed by the patient or their legal representative. It is important to ensure that the document is filled out accurately to avoid any confusion during a medical emergency.
- Healthcare Provider Involvement: A physician must sign the DNR order for it to be valid. Engaging with a healthcare provider can help clarify the implications of the order and ensure that it aligns with the patient’s wishes.
- Communication: It is vital to communicate the existence of the DNR order to family members and healthcare professionals. Keeping copies of the order in accessible locations can help ensure that medical personnel are aware of the patient’s wishes in emergencies.
Common mistakes
Filling out the Pennsylvania Do Not Resuscitate (DNR) Order form is a critical step for individuals who wish to express their preferences regarding medical treatment in emergency situations. However, many people make mistakes that can lead to confusion or unintended consequences. Understanding these common pitfalls can help ensure that your wishes are clearly communicated and respected.
One frequent mistake is failing to provide accurate personal information. It is essential to include your full name, date of birth, and any other identifying details as required. Incomplete or incorrect information can cause delays in honoring your DNR order, potentially putting you at risk during a medical emergency.
Another common error is not having the form properly signed. Both the patient and the physician must sign the DNR order for it to be valid. Some individuals overlook this requirement, thinking that their verbal wishes alone are sufficient. Without the necessary signatures, medical personnel may not recognize the order, leading to unwanted resuscitation efforts.
Many people also forget to discuss their DNR wishes with family members and caregivers. Communication is key. If loved ones are not aware of your decision, they may feel compelled to override your wishes in a moment of crisis. Ensuring that everyone involved in your care understands your preferences can prevent unnecessary stress and confusion.
In addition, neglecting to review and update the DNR order regularly can be problematic. As health conditions change, so too might your preferences regarding resuscitation. Regularly reviewing the form ensures that it reflects your current wishes and medical situation.
Some individuals mistakenly assume that a DNR order is only necessary for terminal illnesses. This misconception can lead to a lack of action when it comes to filling out the form. A DNR order is relevant for anyone who wishes to refuse resuscitation, regardless of their current health status.
Another mistake is not understanding the limitations of the DNR order. While it instructs medical personnel not to perform CPR, it does not affect other forms of medical care. Patients may inadvertently believe that a DNR order means they will receive no medical assistance at all, which is not the case. Clarifying these details with a healthcare provider can help avoid misunderstandings.
Additionally, some people fail to keep copies of their DNR order. It is crucial to have multiple copies accessible to healthcare providers, family members, and caregivers. Without proper documentation readily available, your wishes may not be honored when it matters most.
Lastly, individuals often overlook the importance of consulting with a healthcare professional when completing the DNR order. Guidance from a doctor can provide valuable insight into the implications of the order and help ensure that it aligns with your medical needs and personal values.
By being aware of these common mistakes, individuals can take proactive steps to ensure that their DNR orders are filled out correctly and reflect their true wishes. It is vital to approach this process thoughtfully and with the necessary support.
Misconceptions
- Misconception 1: A Do Not Resuscitate (DNR) order means that a person will not receive any medical care.
- Misconception 2: A DNR order is only for terminally ill patients.
- Misconception 3: A DNR order is permanent and cannot be changed.
- Misconception 4: A DNR order is only valid in hospitals.
- Misconception 5: Completing a DNR order is a complicated process.
This is incorrect. A DNR order specifically addresses resuscitation efforts in the event of cardiac arrest. Other medical treatments and care can still be provided as needed.
While many people with terminal conditions choose to have a DNR, it is not limited to them. Anyone can request a DNR order based on their personal wishes regarding resuscitation.
This is false. A DNR order can be revoked or modified at any time by the patient or their authorized representative, as long as they are able to communicate their wishes.
This is misleading. A DNR order is valid in various settings, including at home and in long-term care facilities, as long as it is properly documented and recognized by the healthcare providers involved.
While it may seem daunting, completing a DNR order is relatively straightforward. Patients can discuss their wishes with their healthcare provider, who can guide them through the necessary steps.
Dos and Don'ts
When filling out the Pennsylvania Do Not Resuscitate Order form, it is important to approach the task with care and attention. Below are some guidelines on what to do and what to avoid.
- Do ensure you understand the implications of a Do Not Resuscitate Order. This decision can have significant consequences for your medical care.
- Do involve your healthcare provider in the process. They can provide valuable insights and help clarify any questions you may have.
- Do discuss your wishes with family members. Open communication can help prevent misunderstandings in the future.
- Do complete the form accurately. Double-check all information to ensure that it reflects your intentions clearly.
- Do keep a copy of the completed form in an accessible place. This ensures that your wishes can be honored when necessary.
- Don't rush through the form. Take your time to consider each section and what it means for your care.
- Don't fill out the form without guidance if you are unsure. Seek help from a medical professional or legal advisor.
- Don't assume your wishes are known by family or healthcare providers. Always document your decisions clearly.
- Don't forget to review the form periodically. Your preferences may change over time, and it is important to keep the document updated.
- Don't neglect to inform your healthcare team about the existence of the Do Not Resuscitate Order. They need to be aware of your wishes.
Browse Popular Do Not Resuscitate Order Forms for US States
What Are Dnr Papers - A DNR order must be easily accessible to ensure that it can be honored in emergency situations.
The Affidavit of Death form is a crucial document that assists in the transition of assets following an individual’s passing. It is essential for those managing estate affairs and is commonly required in various legal contexts. For more information, you can refer to the essential Affidavit of Death form requirements.
Dnr Paperwork - In some situations, advance planning with DNR orders can provide relief and comfort for families.
Dnr Form Ohio - Many patients find peace in knowing their desires regarding resuscitation are formally recorded.
Detailed Guide for Writing Pennsylvania Do Not Resuscitate Order
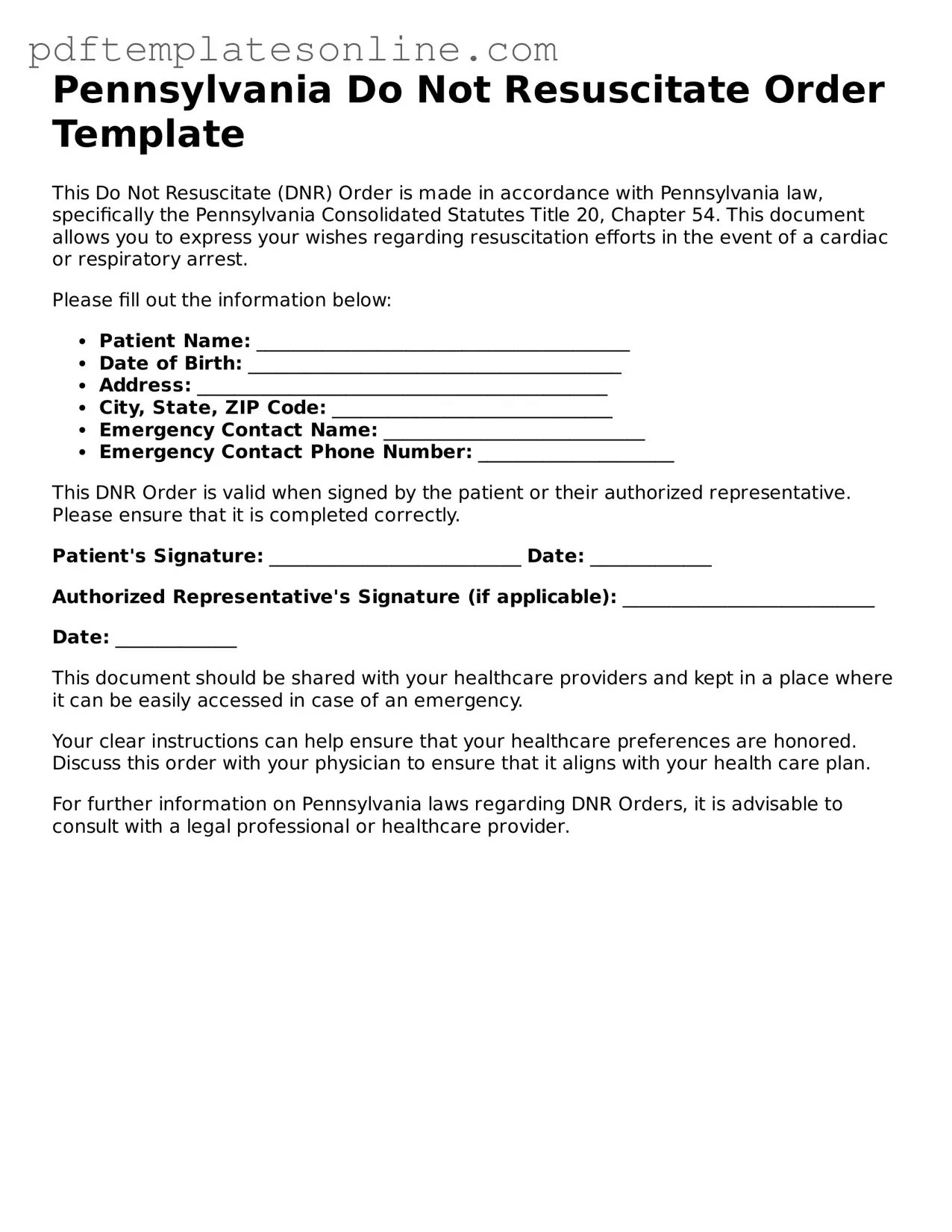
Completing the Pennsylvania Do Not Resuscitate Order form is an important step in ensuring your healthcare preferences are respected. After filling out the form, you will need to keep it in a safe place and share copies with your healthcare providers and family members. Here’s how to fill out the form:
- Obtain the Pennsylvania Do Not Resuscitate Order form. You can find it online or request a copy from your healthcare provider.
- Start with your personal information. Fill in your full name, date of birth, and address at the top of the form.
- Designate a healthcare representative. Write down the name and contact information of the person you trust to make medical decisions on your behalf.
- Specify your wishes. Clearly indicate your desire for a Do Not Resuscitate order by checking the appropriate box on the form.
- Sign and date the form. Make sure to sign your name and write the date on which you are completing the form.
- Have the form witnessed. You will need to have at least one witness sign the form, confirming that you are the person who signed it.
- Make copies. Once the form is complete, make several copies to distribute to your healthcare providers and family members.