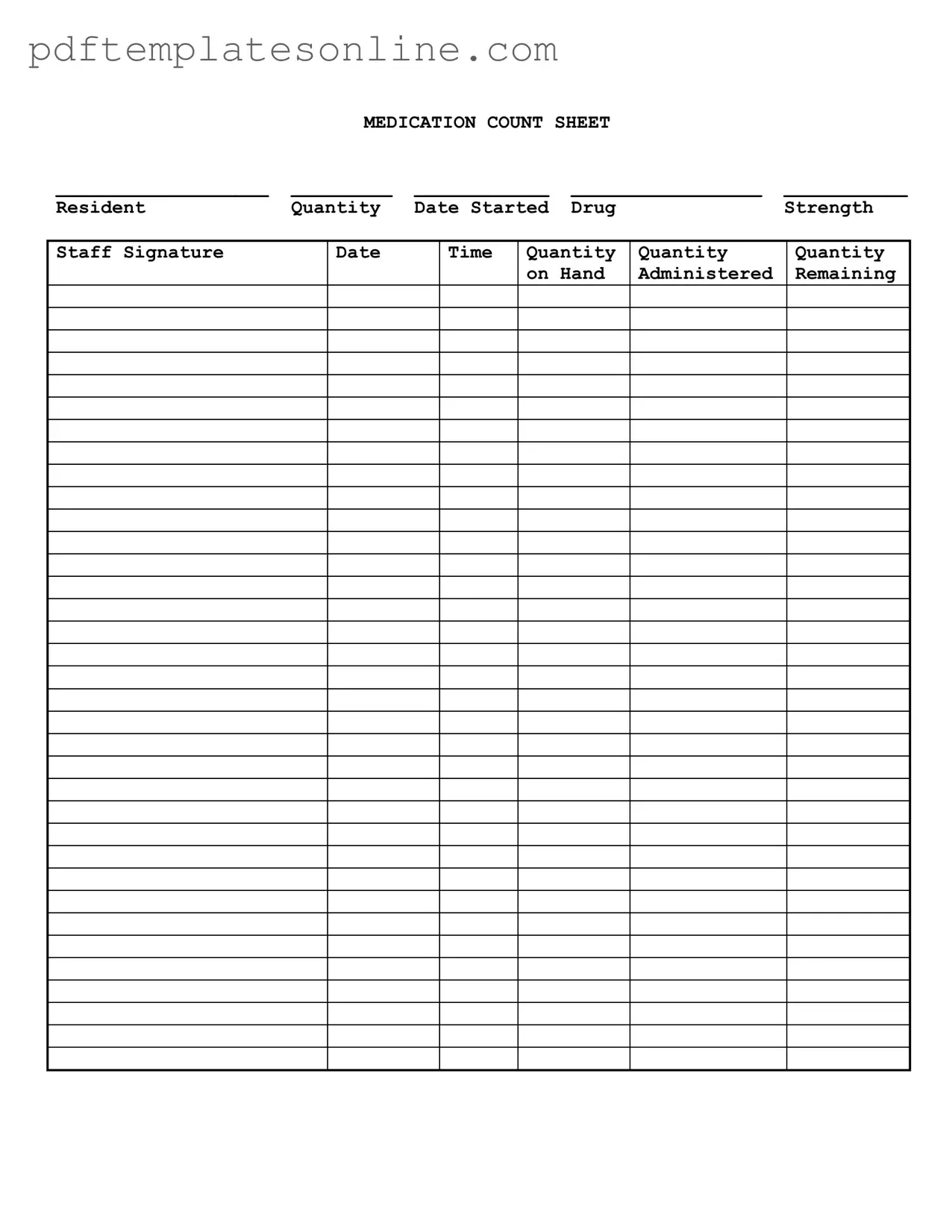
Blank Medication Count Sheet Form
Key takeaways
When it comes to managing medications, a Medication Count Sheet is an essential tool for ensuring accuracy and accountability. Here are some key takeaways to keep in mind while filling out and utilizing this form:
- Accuracy is Crucial: Always double-check the quantities recorded on the sheet. Errors can lead to serious consequences for residents.
- Document Everything: Every entry should include the date, time, and staff signature. This creates a clear trail of accountability.
- Regular Updates: Update the sheet immediately after administering medication. This helps maintain an accurate count and prevents discrepancies.
- Strength Matters: Ensure that the drug strength is clearly noted. This is vital for both safety and proper dosage management.
- Monitor Remaining Quantities: Keep a close eye on the remaining quantities. If supplies are running low, it’s important to reorder in a timely manner.
- Training is Key: All staff members should be trained on how to properly fill out and use the Medication Count Sheet. Consistency in handling this form is essential for effective medication management.
By following these guidelines, you can help ensure that medication management processes are both safe and efficient.
Common mistakes
Filling out the Medication Count Sheet form accurately is crucial for ensuring proper medication management. However, many people make common mistakes that can lead to serious issues. One frequent error is failing to include the resident's name at the top of the form. Without this essential information, it becomes difficult to track which medications belong to which individual, potentially leading to medication errors.
Another common mistake is neglecting to record the date started for each medication. This detail is important for understanding the duration of treatment and for monitoring any changes in the resident's condition. Omitting this information can create confusion and complicate care decisions.
Some individuals forget to note the drug strength on the form. This is a critical piece of information. If the strength is not documented, it can lead to incorrect dosages being administered. Accurate recording helps ensure that residents receive the correct medication at the appropriate strength.
In addition, people often make errors when entering quantities. For instance, they might miscalculate the amount of medication administered or the remaining quantity on hand. These mistakes can have serious implications for patient safety. Double-checking these numbers before finalizing the form can prevent such errors.
Another oversight is failing to obtain the staff signature. The signature serves as verification that the medication has been administered as documented. Without it, there is no accountability, and this can lead to disputes about whether the medication was given.
Many individuals also overlook the importance of recording the date and time of administration. This information is vital for tracking when medications are given and for ensuring that they are administered on schedule. Missing this detail can disrupt medication regimens and affect patient health.
Some people do not update the form promptly. Delays in recording information can lead to inaccuracies. It is essential to fill out the Medication Count Sheet immediately after administering medication to maintain accurate records.
Another mistake involves using abbreviations or unclear handwriting. This can lead to misunderstandings about medication instructions. Clear, legible writing is essential to ensure that everyone involved in the resident's care understands the information provided.
Lastly, failing to review the completed form before submission can lead to overlooked errors. Taking a moment to double-check the entire form can catch mistakes before they become problematic. Attention to detail in completing the Medication Count Sheet is vital for effective medication management and resident safety.
Misconceptions
The Medication Count Sheet form is an essential tool for tracking medication administration in healthcare settings. However, several misconceptions can lead to confusion. Here are four common misunderstandings:
- Misconception 1: The form is only for controlled substances.
- Misconception 2: Staff signatures are optional.
- Misconception 3: The form is only completed at the end of the shift.
- Misconception 4: The count of remaining medication is not important.
Many believe that the Medication Count Sheet is only necessary for tracking controlled substances. In reality, it is used for all medications administered to residents, ensuring accurate records for both controlled and non-controlled drugs.
Some may think that staff signatures are not crucial. However, each entry must be signed by the administering staff to maintain accountability and traceability in medication management.
It is a common belief that the Medication Count Sheet should only be filled out at the end of a shift. In fact, it should be updated continuously throughout the shift to reflect real-time medication administration and inventory levels.
Some may underestimate the importance of tracking remaining medication. Accurate counts are vital for preventing medication errors and ensuring that residents receive the correct dosages as prescribed.
Dos and Don'ts
When filling out the Medication Count Sheet form, it's important to follow certain guidelines to ensure accuracy and compliance. Here’s a list of things you should and shouldn’t do:
- Do double-check the resident's name and medication details before starting.
- Do fill in the quantity clearly, using numbers that are easy to read.
- Do include the date the medication was started to keep track of usage.
- Do sign your name and include the time when you administer the medication.
- Don't leave any sections blank; every field must be filled out.
- Don't use abbreviations that could lead to confusion.
- Don't forget to update the quantity on hand after administration.
- Don't use corrections fluid; if you make a mistake, cross it out neatly and initial it.
Other PDF Forms
Roof Inspection Report Template - Assess the condition of windows near the roof area.
By utilizing resources such as California PDF Forms, individuals can easily access the necessary Living Will form to express their healthcare preferences and ensure that their end-of-life wishes are clearly documented and respected.
Vics Bol - The VICS Bol form streamlines shipping documentation.
Detailed Guide for Writing Medication Count Sheet
Completing the Medication Count Sheet form accurately is essential for maintaining proper medication management. Follow these steps carefully to ensure that all required information is recorded correctly.
- Start by entering the Resident name at the top of the form.
- In the next field, write the Quantity of medication being counted.
- Fill in the Date Started for the medication.
- Next, indicate the Drug name being recorded.
- Write the Strength of the medication next to the drug name.
- In the Staff Signature section, the staff member responsible for the count should sign their name.
- Record the Date of the count.
- Fill in the Time the count was conducted.
- Document the Quantity on Hand before administration.
- Enter the Quantity Administered during this count.
- Finally, calculate and write the Remaining quantity after administration.