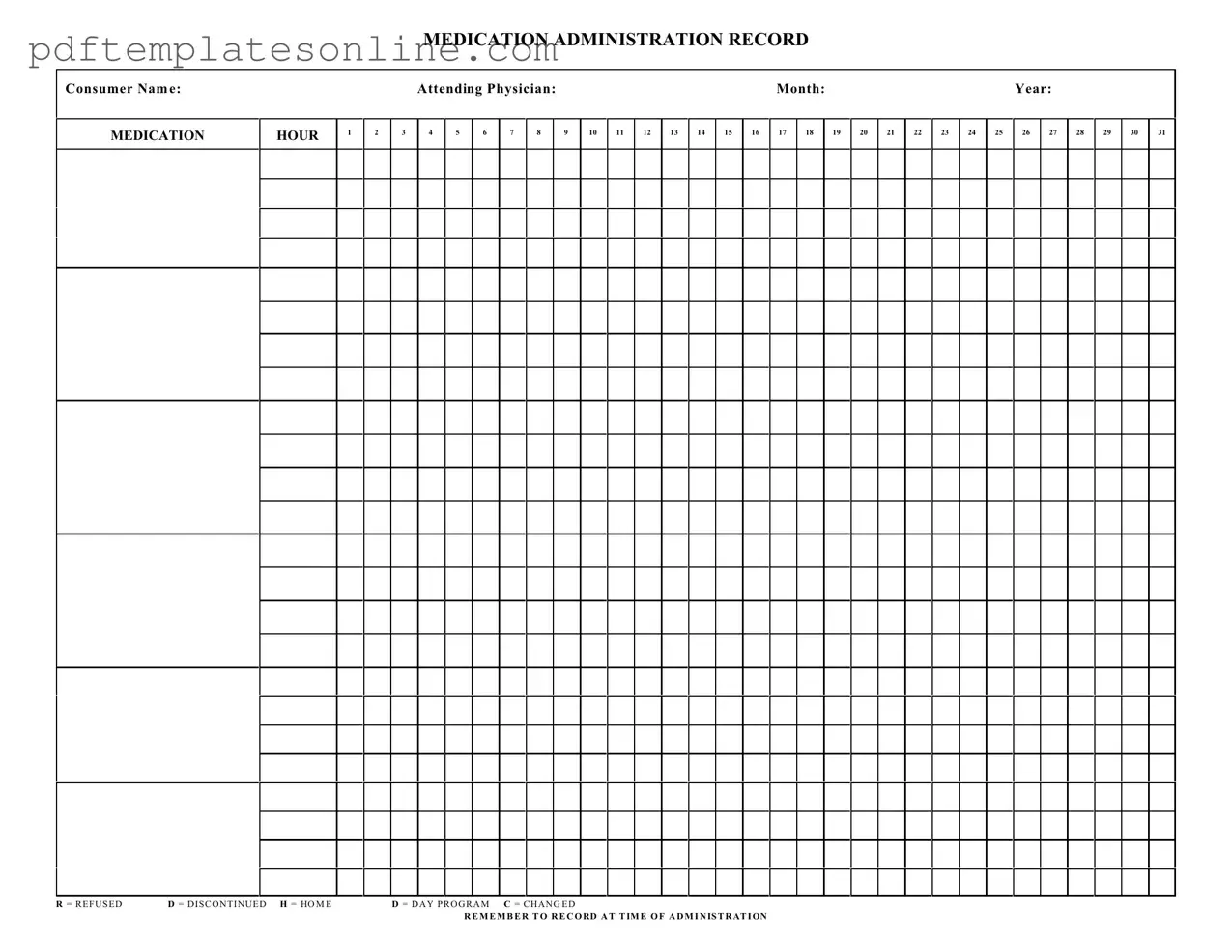
Blank Medication Administration Record Sheet Form
Key takeaways
When using the Medication Administration Record Sheet form, it is important to keep several key points in mind.
- Complete Consumer Information: Always fill in the consumer's name at the top of the form.
- Specify the Attending Physician: Include the name of the physician responsible for the consumer's care.
- Record the Month and Year: Clearly indicate the month and year for which the medications are being administered.
- Use Accurate Medication Hours: Mark the appropriate hour for each medication dose as specified on the form.
- Indicate Refusals and Changes: Use the designated codes (R, D, H, C) to note if a medication was refused, discontinued, or changed.
- Document at Administration Time: Always record the information at the time of administration to ensure accuracy.
- Track Daily Program Medications: Be mindful of medications that are specific to day programs or home settings.
- Maintain Clarity: Write legibly to avoid any confusion about medication details.
- Review Regularly: Regularly review the record to ensure all entries are complete and accurate.
- Follow Up on Changes: If a medication is changed, ensure that the new information is documented promptly.
Common mistakes
Filling out the Medication Administration Record Sheet can be a straightforward task, but mistakes often occur. One common error is failing to include the consumer's name. Without this crucial information, it becomes impossible to track which individual received the medication. Always ensure that the name is clearly written at the top of the form.
Another frequent mistake is neglecting to record the attending physician's name. This detail is important for accountability and communication. If a question arises about the medication, knowing who prescribed it can streamline the process of obtaining clarification.
Many people also forget to fill in the month and year on the form. This oversight can lead to confusion about when the medications were administered. Always double-check that these fields are completed to maintain accurate records.
Inaccurate recording of the medication hours is another common issue. Each hour should be clearly marked to indicate when the medication was given. Missing or incorrect times can cause serious medication errors and affect the consumer's health.
Some individuals mistakenly use abbreviations or codes that are not universally understood. For instance, marking "D" for discontinued without explaining what it means can lead to misinterpretation. It is best to use clear language to ensure everyone understands the information on the record.
Another error involves not recording whether the medication was refused or changed. If a consumer refuses medication, it must be documented at the time of administration. Likewise, any changes to the medication regimen should be noted immediately to avoid confusion later.
People sometimes forget to sign or date the record after completing it. This step is essential for verifying that the medication was administered as prescribed. Always include your signature and the date to provide a complete and accurate record.
Lastly, many fail to review the completed form for accuracy. Taking a moment to check for any mistakes can prevent significant issues down the line. Regular audits of the Medication Administration Record Sheet can help catch errors and improve the overall process.
Misconceptions
Misconceptions about the Medication Administration Record Sheet can lead to confusion and errors in medication management. Here are five common misunderstandings:
- It is only for nurses to use. Many believe that only nurses can fill out the Medication Administration Record Sheet. In reality, any qualified healthcare provider involved in medication administration can use it. This includes pharmacists and trained caregivers.
- It does not need to be updated regularly. Some think that once the Medication Administration Record is filled out, it remains static. However, it is crucial to update the record whenever there are changes in medication, dosages, or patient status to ensure accuracy.
- Refusal of medication can be ignored. A common misconception is that if a patient refuses medication, it does not need to be documented. In fact, any refusal must be recorded immediately to maintain a clear medical history and to inform future care decisions.
- All medications are recorded on the same line. Many people assume that all medications can be listed on a single line. However, each medication should be documented separately to avoid confusion and ensure clarity in administration.
- Recording is only necessary at the end of the day. Some believe that they can wait until the end of the day to complete the record. In truth, it is essential to record medications at the time of administration to prevent errors and ensure patient safety.
Dos and Don'ts
When filling out the Medication Administration Record Sheet form, consider the following guidelines:
- Do write clearly and legibly to ensure all information is easily readable.
- Do record the consumer's name and attending physician accurately.
- Do document the date and time of medication administration promptly.
- Do use the appropriate codes for refused or discontinued medications.
- Don't leave any sections blank; fill in all required fields completely.
- Don't use abbreviations that may be unclear or misinterpreted.
Other PDF Forms
I-120 - It contains critical details about the student's program of study.
Fillable Da Form 638 - The DA 638 can be used for both live individuals and posthumous nominations.
When navigating the complex process of real estate transactions, utilizing resources such as the California PDF Forms can greatly aid buyers and sellers in creating a comprehensive and legally binding agreement, ensuring that all essential details are clearly specified within the document.
Printable:5s6uydlipco= Living Will Template - Five Wishes gives voice to those who may not be able to speak for themselves.
Detailed Guide for Writing Medication Administration Record Sheet
Filling out the Medication Administration Record Sheet is a straightforward process that ensures accurate tracking of medication administration. Following these steps will help maintain clarity and consistency in documenting medication details.
- Begin by entering the Consumer Name at the top of the form.
- Next, write the Attending Physician's Name in the designated space.
- Fill in the Month and Year for the record.
- For each medication administration, identify the Medication Hour by marking the appropriate hour column.
- Record the date by marking the corresponding day in the calendar section.
- In the event of a refused medication, write R in the appropriate box; for discontinued medication, use D; for home administration, use H; for day program, use D; and if there was a change, mark C.
- Always remember to record at the time of administration to ensure accuracy.