Official Georgia Do Not Resuscitate Order Document
Key takeaways
When considering the Georgia Do Not Resuscitate (DNR) Order form, it is essential to understand its purpose and the implications it carries. Below are key takeaways to keep in mind.
- The DNR Order allows individuals to express their wishes regarding resuscitation in the event of a medical emergency.
- It is crucial to have the DNR Order signed by a physician to ensure it is valid and recognized by healthcare providers.
- The form must be readily accessible to medical personnel, ideally kept in a location where it can be easily found, such as on the refrigerator or with other important medical documents.
- Individuals should discuss their DNR wishes with family members and caregivers to ensure everyone understands their preferences.
- Regularly reviewing and updating the DNR Order is important, especially if there are changes in health status or personal preferences.
- In Georgia, a DNR Order is legally binding and must be honored by healthcare providers, reflecting the individual’s wishes regarding end-of-life care.
Understanding these key aspects of the Georgia DNR Order can help ensure that personal healthcare preferences are respected and upheld during critical moments.
Common mistakes
Completing a Do Not Resuscitate (DNR) Order form in Georgia is a significant decision that requires careful consideration. However, many individuals make common mistakes that can lead to confusion or complications. Understanding these pitfalls can help ensure that the form accurately reflects one's wishes.
One frequent error is failing to provide complete personal information. The DNR form requires the full name, date of birth, and signature of the individual making the request. Omitting any of these details can render the document invalid. Additionally, it's essential to include the signature of a witness, as this adds credibility to the document.
Another common mistake is not discussing the decision with family members or healthcare providers. A DNR order can have significant implications for medical treatment. By having open conversations, individuals can ensure their loved ones understand their wishes, reducing potential conflict during critical moments.
Some people mistakenly assume that a DNR order is permanent and cannot be changed. In reality, individuals have the right to revoke or modify their DNR orders at any time. This flexibility allows for adjustments as personal circumstances or health conditions change.
Moreover, individuals sometimes overlook the importance of ensuring that the DNR form is easily accessible. If the document is stored away in a drawer or a folder, medical personnel may not be able to locate it when needed. Keeping a copy in a visible place, such as on the refrigerator or with medical records, can help ensure that it is readily available in an emergency.
Additionally, people may forget to review the form periodically. As life circumstances evolve, so too may a person's preferences regarding medical care. Regularly checking the DNR order ensures that it remains aligned with current wishes.
Another mistake involves misunderstanding the scope of the DNR order. Some individuals may incorrectly believe that a DNR order means that all medical treatment will be withheld. In fact, a DNR specifically addresses resuscitation efforts and does not affect other forms of care. Clarifying this distinction is crucial for both the individual and their healthcare providers.
Failing to consult legal or medical professionals can also lead to errors. While the DNR form is designed to be straightforward, seeking guidance can help clarify any uncertainties and ensure that the form complies with state laws.
Furthermore, individuals might neglect to inform their healthcare team about the existence of the DNR order. Communication with doctors and nurses is vital to ensure that everyone involved in a person's care is aware of their wishes. This can prevent misunderstandings and ensure that the individual's preferences are honored.
Lastly, some individuals may be hesitant to complete a DNR order due to fear or stigma associated with end-of-life discussions. However, taking the time to understand and complete the form can provide peace of mind, knowing that one's wishes are documented and respected.
Misconceptions
Understanding the Georgia Do Not Resuscitate (DNR) Order form is crucial for individuals and families making important healthcare decisions. However, several misconceptions often arise regarding this document. Below is a list of common misunderstandings.
- A DNR means no medical care will be provided. This is not true. A DNR specifically instructs medical personnel not to perform CPR in the event of cardiac arrest. Other medical treatments and interventions can still be administered.
- Only terminally ill patients need a DNR. While many people with terminal illnesses choose to have a DNR, anyone can request one based on their personal healthcare wishes, regardless of their current health status.
- A DNR is only valid in hospitals. This is a misconception. A properly executed DNR is valid in all healthcare settings, including at home, nursing homes, and during emergency situations.
- Once signed, a DNR cannot be changed or revoked. This is incorrect. Individuals can change or revoke a DNR at any time, provided they communicate their wishes clearly to healthcare providers.
- A DNR form is the same as an advance directive. While both documents relate to end-of-life care, they serve different purposes. An advance directive outlines broader healthcare preferences, while a DNR specifically addresses resuscitation efforts.
- Having a DNR means giving up on life. Many people view a DNR as a way to maintain dignity and avoid unnecessary suffering. It is a personal choice that reflects individual values regarding end-of-life care.
Clarifying these misconceptions can help individuals and families make informed decisions about their healthcare preferences. It is always advisable to discuss these matters with a healthcare professional.
Dos and Don'ts
When filling out the Georgia Do Not Resuscitate (DNR) Order form, it’s important to follow certain guidelines to ensure that your wishes are clearly communicated. Here’s a list of what to do and what to avoid:
- Do ensure that the form is completed in full, including all required signatures.
- Do discuss your wishes with your healthcare provider and family members.
- Do keep a copy of the completed form in an easily accessible location.
- Do review the form periodically to ensure it still reflects your wishes.
- Do consult legal advice if you have questions about the implications of the DNR order.
- Don't sign the form without fully understanding its contents.
- Don't assume that verbal instructions are sufficient; always use the official form.
- Don't forget to notify your healthcare team that you have a DNR order in place.
- Don't leave the form in a place where it might be overlooked in an emergency.
- Don't hesitate to update the form if your health status or preferences change.
Browse Popular Do Not Resuscitate Order Forms for US States
Dnr Form Ohio - The presence of a DNR order does not affect other aspects of medical treatment and care.
What Are Dnr Papers - Individuals can use a Do Not Resuscitate Order to avoid unwanted medical interventions during terminal illness.
Dnr Paperwork - Keeping a copy of the DNR in a visible location, such as on the fridge or next to the bed, is advisable.
A Living Will form, specifically in California, is a legal document that lets people state their wishes for end-of-life medical care, in case they become unable to communicate their decisions. It's a way to ensure that one's healthcare preferences are known and respected. For further assistance in creating this important document, you can check out California PDF Forms. Understanding this form is crucial for anyone looking to have control over their medical treatment options.
Texas Dnr Law - Implementing a DNR can provide families with clarity and reduce stress during difficult medical decisions.
Detailed Guide for Writing Georgia Do Not Resuscitate Order
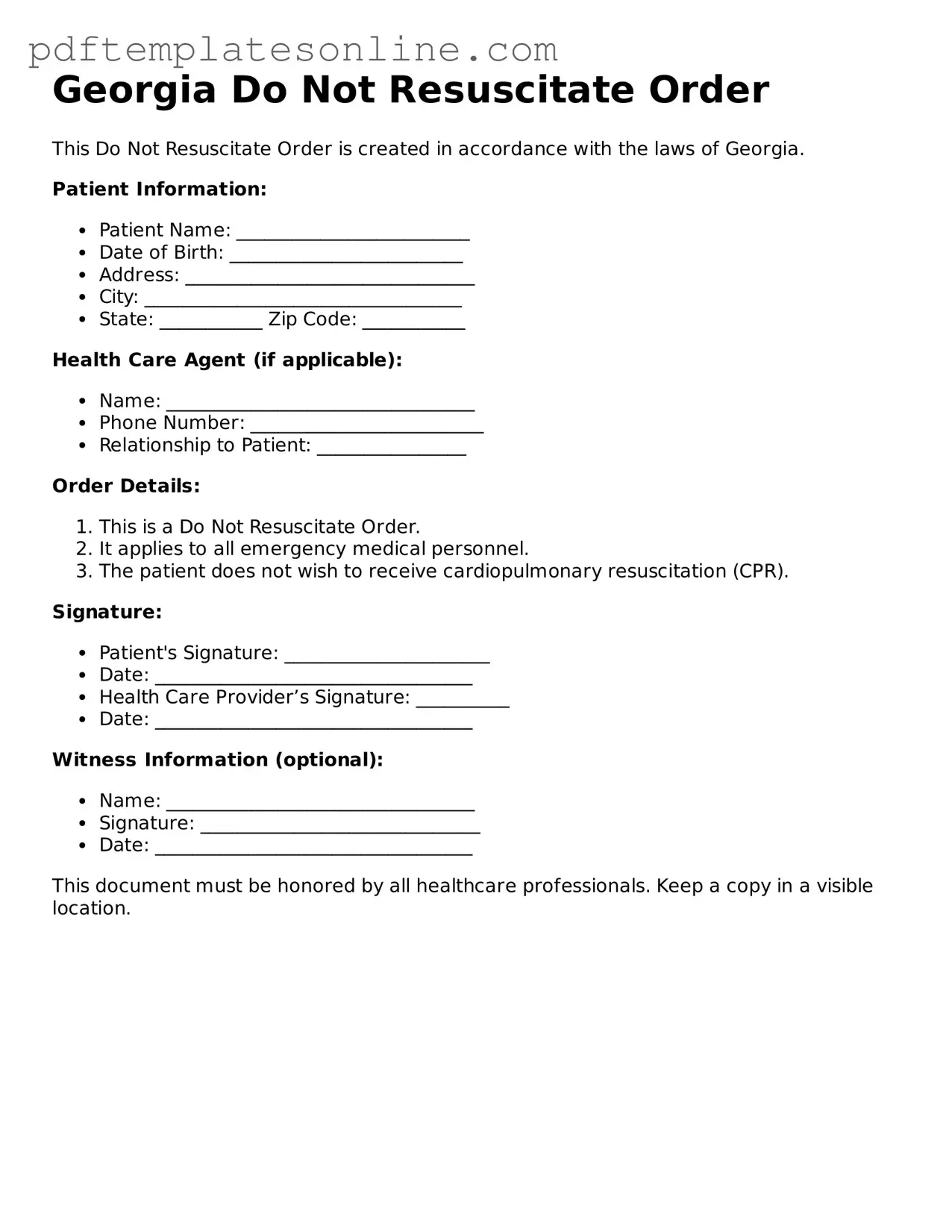
Completing the Georgia Do Not Resuscitate Order form is an important step in expressing your healthcare wishes. This document will help ensure that your preferences regarding resuscitation efforts are known and respected by medical personnel. Here’s how to fill it out properly.
- Start by downloading the Georgia Do Not Resuscitate Order form from a reliable source, such as the Georgia Department of Public Health website.
- Read through the instructions carefully to understand what information is required.
- In the designated section, fill in your full name, date of birth, and any other personal identifying information requested.
- Provide the name of your physician. This is important, as the order must be signed by a licensed physician.
- Clearly indicate your wishes regarding resuscitation by checking the appropriate boxes. Make sure to review the options thoroughly.
- Sign and date the form in the space provided. Your signature is crucial for the document to be valid.
- If you have a witness, they should sign the form as well. Ensure that the witness is not a family member or your healthcare provider.
- Make copies of the completed form for your records and to share with your healthcare providers.
- Keep the original form in a safe but accessible location, so it can be easily found when needed.
Once you have filled out the form, it is essential to discuss your decisions with your family and healthcare team. Open conversations about your choices can provide clarity and support for everyone involved.