Blank Cna Shower Sheets Form
Key takeaways
Here are some key takeaways regarding the use of the CNA Shower Sheets form:
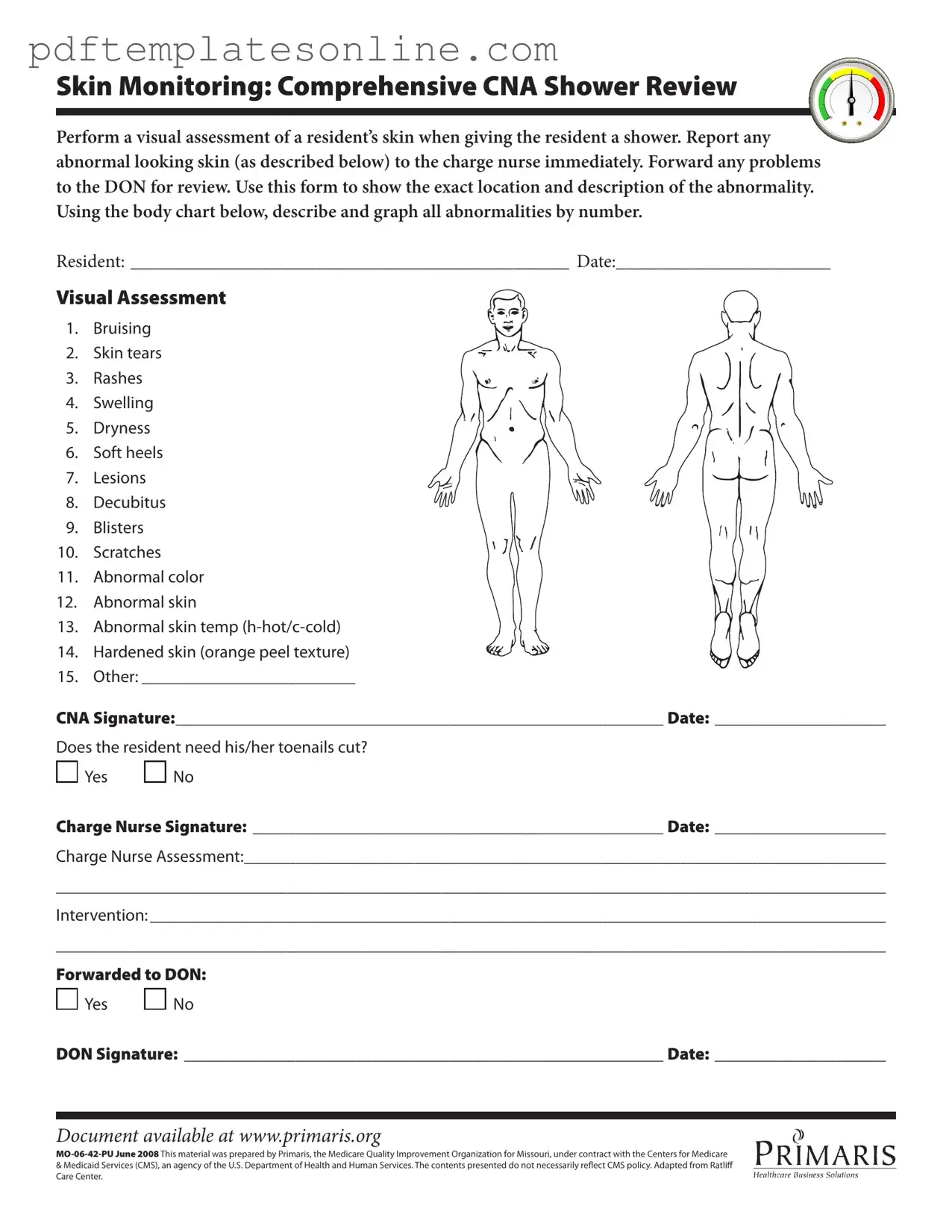
- Visual Assessment is Crucial: Conduct a thorough visual assessment of the resident's skin during showers. This helps in identifying any abnormalities that may need immediate attention.
- Report Abnormalities Promptly: Any unusual findings, such as bruises or skin tears, must be reported to the charge nurse without delay. Quick action can prevent further complications.
- Document Accurately: Use the form to accurately describe and graph any abnormalities. Include specific locations and types of issues to ensure clear communication with the healthcare team.
- Follow Up with Higher Authority: If necessary, forward any concerns to the Director of Nursing (DON) for further review. This ensures that all issues are addressed appropriately.
Common mistakes
Filling out the CNA Shower Sheets form is a critical task that directly impacts the care of residents. However, there are common mistakes that individuals often make, which can lead to miscommunication and inadequate care. One significant error is failing to conduct a thorough visual assessment. It’s essential to carefully examine the resident’s skin for any abnormalities before documenting them. Skipping this step can result in overlooking serious conditions that require immediate attention.
Another frequent mistake involves incomplete or inaccurate descriptions of skin abnormalities. When noting issues like bruising or rashes, it is vital to provide specific details about their location and appearance. For instance, simply stating "there is a rash" does not convey the necessary information. Instead, one should describe the rash's size, color, and any associated symptoms. This level of detail aids healthcare providers in making informed decisions about the resident's care.
People also tend to neglect the importance of using the body chart provided in the form. This chart serves as a visual aid to pinpoint the exact location of skin issues. Failing to utilize it may lead to confusion or misinterpretation of where the problems are located. Properly marking the chart not only enhances clarity but also ensures that the charge nurse and other healthcare professionals understand the situation accurately.
Another common oversight is not reporting abnormalities promptly to the charge nurse. Immediate communication is crucial when it comes to skin issues. Delaying this step can exacerbate the resident's condition and hinder timely interventions. It’s important to remember that timely reporting can significantly improve outcomes for residents with skin concerns.
In addition, some CNAs may forget to sign and date the form after completing their assessments. This signature is not just a formality; it serves as a record of accountability and ensures that there is a clear trail of who conducted the assessment. Omitting this step can create gaps in documentation, which may complicate future care or audits.
Lastly, a mistake that can have serious implications is failing to follow through on interventions or not forwarding the information to the Director of Nursing (DON) when necessary. If a resident requires further evaluation or treatment, it is essential to document that and ensure the DON is aware. Neglecting to do so can leave residents without the appropriate care they need, potentially leading to worsened health outcomes.
Misconceptions
Here are six common misconceptions about the CNA Shower Sheets form:
- It’s only for documenting skin issues. Many believe the form is solely for skin abnormalities, but it also includes sections for toenail care and overall assessments.
- Only the CNA can fill it out. While CNAs complete the initial assessment, the charge nurse and DON also play crucial roles in reviewing and signing off on the form.
- It’s optional to report skin abnormalities. In fact, reporting any abnormal skin condition is mandatory and should be done immediately to ensure proper care.
- All skin issues are the same. The form requires detailed descriptions of various skin conditions, such as bruising and lesions, which can have different implications for treatment.
- It’s not important to document the exact location of issues. Accurate location details are essential for effective monitoring and treatment, making this aspect of the form critical.
- The form is outdated and not useful. The CNA Shower Sheets form is regularly updated to meet current standards and guidelines, ensuring it remains relevant for effective patient care.
Dos and Don'ts
When filling out the CNA Shower Sheets form, it is essential to ensure that the information is accurate and complete. Here are five important dos and don’ts to keep in mind:
- Do perform a thorough visual assessment of the resident's skin during the shower.
- Do report any abnormalities, such as bruising or rashes, to the charge nurse immediately.
- Do accurately describe and graph all abnormalities on the body chart provided.
- Do ensure that all sections of the form are filled out completely, including signatures and dates.
- Do forward any concerns to the Director of Nursing (DON) for further review.
- Don’t overlook any signs of skin issues, even if they seem minor.
- Don’t leave any fields blank; every section is important for proper documentation.
- Don’t use vague descriptions; be specific about the location and nature of any abnormalities.
- Don’t forget to check if the resident needs toenail care, as this is a crucial part of their hygiene.
- Don’t delay in reporting issues; timely communication is vital for resident care.
Other PDF Forms
Da Form 7666 - This document aids in evaluating training readiness of units.
To obtain necessary legal documentation, individuals may find it beneficial to explore this essential resource: the comprehensive Affidavit of Death form, which ensures a smooth transition of property ownership and honors the deceased's legacy.
6 Team Single Elimination Bracket With Consolation - Game 1 kicks off the consolation bracket and sets the tone for the competition.
Detailed Guide for Writing Cna Shower Sheets
Completing the CNA Shower Sheets form requires attention to detail and accuracy to ensure proper documentation of the resident's skin condition. This process involves assessing the resident's skin, noting any abnormalities, and obtaining necessary signatures. Follow the steps outlined below to fill out the form correctly.
- Begin by writing the resident's name in the space labeled RESIDENT:.
- Enter the date of the assessment in the DATE: field.
- Conduct a visual assessment of the resident's skin during the shower.
- Identify any abnormalities from the provided list, such as bruising, rashes, or skin tears.
- Use the body chart included in the form to graphically indicate the location of each abnormality by number.
- In the Other: section, describe any abnormalities not listed.
- Sign the form in the CNA Signature: field and enter the date.
- Determine if the resident needs toenail trimming and mark Yes or No.
- Have the charge nurse sign the form in the Charge Nurse Signature: section and record the date.
- Provide a summary of the charge nurse's assessment in the designated area.
- Outline any interventions taken in the Intervention: section.
- Indicate whether the issue has been forwarded to the Director of Nursing (DON) by marking Yes or No.
- Finally, the DON should sign the form and include the date.