Blank Certification Of Incapacity Form
Key takeaways
When filling out and using the Certification of Incapacity form, consider the following key takeaways:
- Accurate Examination: The attending physician must conduct a thorough examination of the patient to determine their capacity to make informed decisions.
- Clear Documentation: Clearly state the patient's condition and why they are incapable of understanding or communicating decisions regarding medical treatment.
- Timeliness: One of the physician certifications must be completed within two hours of the examination to ensure the validity of the assessment.
- Signature Requirement: Both the attending physician and a second physician must sign the form to confirm their findings and provide necessary validation.
- Check Relevant Boxes: It is essential to check the appropriate boxes regarding the patient's ability to evaluate risks and benefits or communicate decisions.
Common mistakes
Filling out the Certification of Incapacity form can be challenging. One common mistake is failing to provide complete patient information. Both the attending physician and the second physician must clearly identify the patient by name. Missing or incorrect details can lead to confusion and delays in treatment.
Another frequent error is neglecting to check the appropriate box regarding the patient's ability to make decisions. The form requires the physician to specify whether the patient is unable to evaluate treatment options or communicate a decision. Omitting this crucial step may result in misunderstandings about the patient's condition.
Additionally, physicians often forget to sign and date the form properly. Each certification must include the physician's signature, along with the date and time of the examination. Incomplete signatures can render the form invalid, complicating the patient's care process.
Another mistake involves the timing of the certification. The form states that one of the certifications must be made within two hours of examining the patient. Failing to adhere to this requirement can lead to legal complications and may undermine the validity of the certification.
Lastly, some physicians may provide vague or insufficient descriptions of the patient's condition. The form requires a detailed explanation of the patient's incapacity and the specific medical treatments involved. A lack of clarity can create confusion and may not adequately support the need for incapacity certification.
Misconceptions
Misconceptions about the Certification of Incapacity form can lead to confusion and misinterpretation. Here are ten common misconceptions explained:
- The form is only for elderly patients. This form can be used for patients of any age who are unable to make informed decisions due to medical conditions.
- Only one physician's signature is needed. Both an attending physician and a second physician must certify the patient's incapacity to ensure a thorough evaluation.
- The form is permanent. The certification is not permanent. It is specific to the patient's condition at the time of examination and can change.
- Patients cannot regain their decision-making capacity. Patients may recover their ability to make informed decisions as their medical condition improves.
- This form overrides all patient rights. The form does not strip patients of their rights; it simply acknowledges their current incapacity to make informed decisions.
- It is only applicable in emergency situations. The Certification of Incapacity form can be used in both emergency and non-emergency situations when a patient is unable to make decisions.
- Physicians can complete the form without examining the patient. A physical examination is required to assess the patient's condition before completing the certification.
- The form is a legal document and cannot be challenged. The certification can be contested, especially if new evidence arises regarding the patient's capacity.
- Patients must be unconscious to be deemed incapacitated. Incapacity can occur due to various conditions, including severe mental health issues or cognitive impairments, not just unconsciousness.
- The form is only for medical treatment decisions. While it primarily addresses medical treatment, it can also relate to other decisions affected by the patient's incapacity.
Dos and Don'ts
When filling out the Certification of Incapacity form, it is important to follow specific guidelines to ensure accuracy and compliance. Below is a list of ten things to do and not do during this process.
- Do clearly state the patient's name and details in the designated areas.
- Do provide the date and time of the examination accurately.
- Do describe the patient's condition in detail to support your findings.
- Do check one of the boxes regarding the patient's ability to evaluate treatment options.
- Do ensure that the attestation is made within two hours of the examination.
- Don't leave any sections of the form blank; complete all required fields.
- Don't use vague language; be specific about the patient's incapacity.
- Don't forget to sign and date the form after completing it.
- Don't provide information that is not relevant to the patient's incapacity.
- Don't alter the form in any way; use it as it is provided.
Other PDF Forms
Aspen Dental Health Information Release - Revoking permission must be done in writing to Aspen Dental.
The EDD DE 2501 form is a document used in California to apply for state disability insurance benefits. It provides essential information about the applicant's medical condition and work history. Understanding how to complete this form accurately is crucial for securing the financial support you may need during a period of temporary disability. For more details and resources, you can visit https://mypdfform.com/blank-edd-de-2501.
What Is a Ub-04 Form - Updates to personal information can be made directly on this form.
Status Change Form - Document compliance status for an employee in training.
Detailed Guide for Writing Certification Of Incapacity
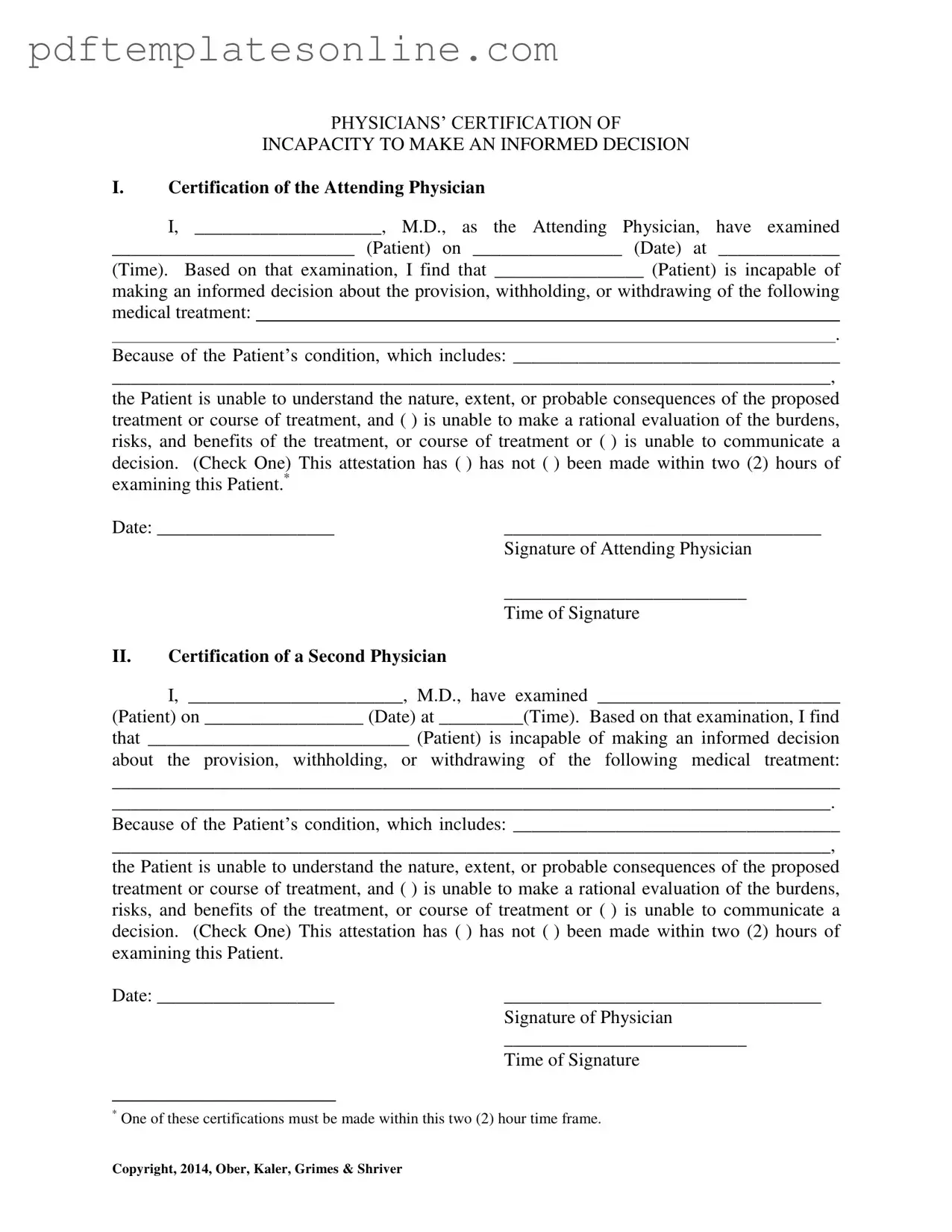
After completing the Certification of Incapacity form, it will be submitted to the appropriate medical or legal authority for review. This form requires signatures from two physicians to validate the patient's incapacity to make informed medical decisions. Below are the steps to fill out the form accurately.
- Begin with the first section titled "Certification of the Attending Physician."
- In the first blank, write the name of the attending physician.
- Fill in the patient's name in the next blank.
- Enter the date of examination in the designated space.
- Provide the time of the examination.
- State the specific medical treatment the patient is incapable of making decisions about.
- Describe the patient's condition in detail, explaining why they cannot understand the treatment options.
- Check one of the boxes to indicate whether the patient is unable to make a rational evaluation of the treatment or unable to communicate a decision.
- Indicate whether the attestation was made within two hours of the examination by checking the appropriate box.
- Write the date of attestation.
- Have the attending physician sign the form and write their time of signature.
- Move to the second section titled "Certification of a Second Physician."
- Repeat steps 2 through 11 for the second physician, ensuring all information is filled out accurately.