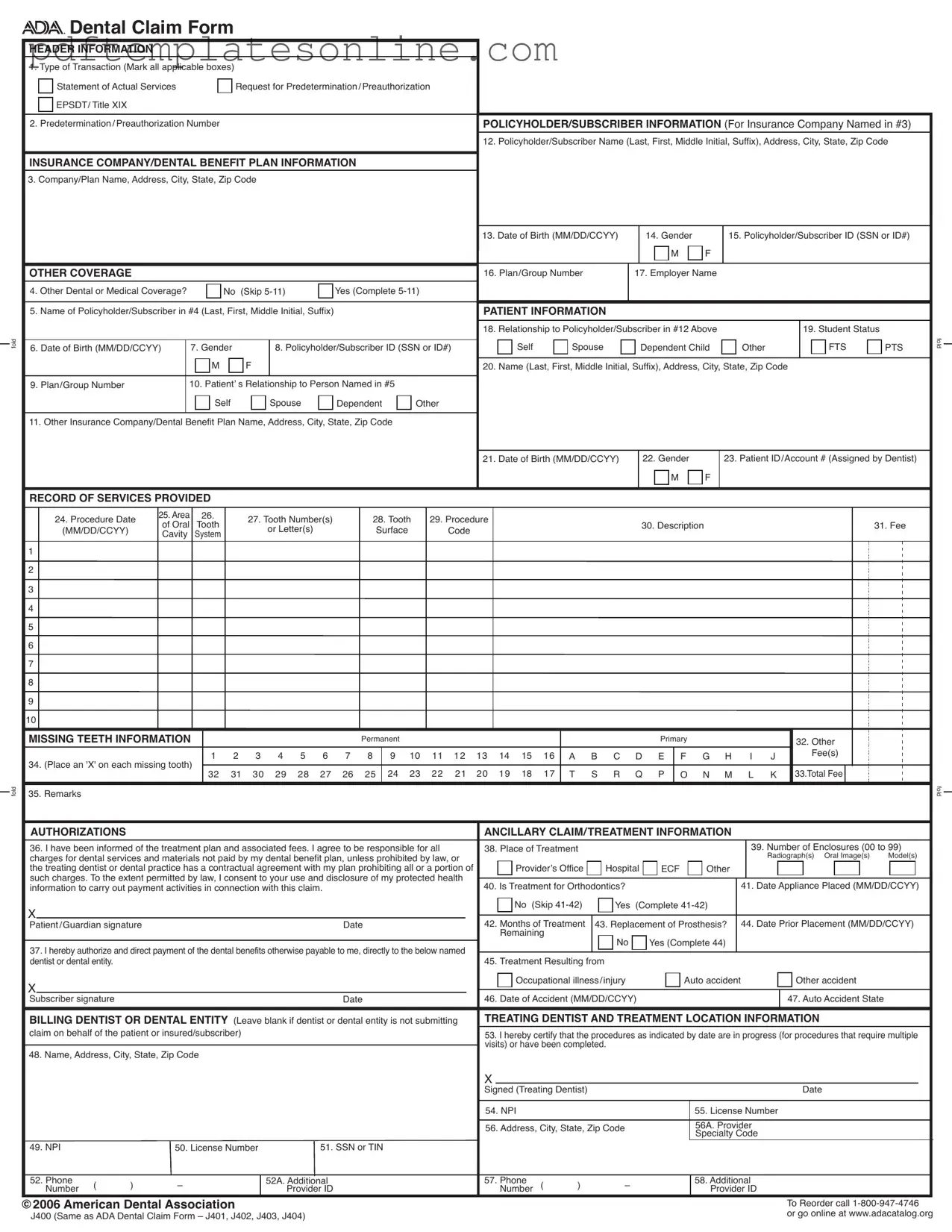
Blank Ada Dental Claim Form
Key takeaways
Filling out the ADA Dental Claim Form accurately is essential for timely processing of claims. Here are key takeaways to consider:
- Type of Transaction: Indicate all applicable transaction types at the top of the form.
- Policyholder Information: Provide complete details for the policyholder, including name, address, and date of birth.
- Insurance Information: Clearly enter the insurance company’s name and address, ensuring it is visible for processing.
- Other Coverage: If there is additional dental or medical coverage, complete the relevant sections.
- Patient Information: Fill out the patient’s relationship to the policyholder and their personal details accurately.
- Record of Services: Document each procedure with the corresponding date, tooth number, and fee.
- Missing Teeth: Mark any missing teeth on the form to avoid confusion during claim processing.
- Authorization: Ensure that the patient or guardian signs the authorization section to allow for payment processing.
- Coordination of Benefits: Attach the primary payer’s Explanation of Benefits (EOB) when submitting to a secondary payer.
- National Provider Identifier: Include the NPI for both the treating dentist and the billing entity, if applicable.
Following these guidelines will help facilitate the claims process and ensure that all necessary information is included for review.
Common mistakes
Filling out the ADA Dental Claim Form can seem straightforward, yet many individuals encounter common pitfalls that can lead to delays or denials of claims. One frequent mistake is failing to complete all required fields. Each section of the form has specific information that must be provided. Omitting even a single detail, such as the policyholder's date of birth or the patient's relationship to the policyholder, can result in processing issues.
Another common error occurs when individuals neglect to provide accurate information regarding the insurance company. The name and address of the insurance provider must be clearly filled out in the designated area. If this information is incorrect or incomplete, the claim may not reach the appropriate payer, leading to unnecessary complications.
People often overlook the importance of the procedure date. Each service must be accompanied by the correct date, formatted as MM/DD/YYYY. Incorrectly formatted dates or missing dates can lead to confusion and potential rejection of the claim.
Additionally, many individuals fail to provide the National Provider Identifier (NPI) for the treating dentist. This unique identifier is crucial for ensuring that claims are processed correctly. Without it, the claim may be delayed or returned for further information.
Another mistake is not indicating the patient’s relationship to the policyholder. This detail is essential for verifying coverage and ensuring that the claim is processed under the correct insurance plan. Mislabeling this relationship can lead to significant delays in payment.
Moreover, individuals sometimes neglect to sign the form. A signature is required to authorize the release of information and the payment of benefits. Without this signature, the claim cannot be processed, and the patient may face unexpected charges.
Inaccurate or incomplete fee entries also pose a challenge. Each procedure must have an associated fee, clearly indicated. If the fees are not properly recorded, it may lead to discrepancies between the services provided and the amount billed, resulting in potential disputes.
Finally, failing to attach necessary documentation can hinder the claim process. If the claim involves coordination of benefits, the Explanation of Benefits (EOB) from the primary payer must be included. Neglecting to do so can result in the claim being denied or delayed as the insurance company seeks additional information.
Misconceptions
Here are some common misconceptions about the ADA Dental Claim Form:
- All fields must be filled out completely. While it is important to provide as much information as possible, not every field is mandatory. Check the form for specific instructions on which fields can be left blank.
- The form is only for dental insurance claims. This form can also be used for predetermination or preauthorization requests, not just for submitting claims after treatment.
- Only the dentist can submit the form. Patients or guardians can submit the claim as well, provided they have the necessary information and signatures.
- Missing teeth do not need to be reported. It is essential to indicate any missing teeth on the form, as this can affect the coverage and payment from the insurance provider.
- The date format is flexible. All dates must be entered in the MM/DD/YYYY format. Ensure you follow this format to avoid processing delays.
- Submitting multiple procedures requires multiple forms. If there are more procedures than available lines on one form, you can list additional procedures on a separate, fully completed claim form.
- All dental providers have the same identification number. Each dental provider has a unique National Provider Identifier (NPI) or other identifiers. Make sure to enter the correct one for accurate processing.
Dos and Don'ts
When filling out the ADA Dental Claim Form, it's essential to ensure accuracy and completeness. Below is a list of things you should and shouldn't do to help streamline the process.
- Do read the instructions carefully before starting.
- Do fill in all required fields completely.
- Do use clear and legible handwriting or type the information.
- Do double-check the policyholder's information for accuracy.
- Do include the correct dates in the MM/DD/YYYY format.
- Don't leave any mandatory fields blank.
- Don't forget to include the patient's relationship to the policyholder.
- Don't use abbreviations or shorthand that could cause confusion.
- Don't forget to sign and date the form where required.
- Don't submit the claim without attaching any necessary documentation, like the primary payer’s Explanation of Benefits.
By following these guidelines, you can help ensure that your dental claim is processed smoothly and efficiently.
Other PDF Forms
Emergency Leave - Returning from leave must be done at or before your normal workday start to avoid charges.
For those looking to create or understand a California Non-compete Agreement form, utilizing resources such as California PDF Forms can provide valuable insights and templates. This is essential for ensuring compliance with state laws while addressing the nuances that come with these agreements, especially since they are often unenforceable in California, making awareness critical for employers and employees alike.
Transfer of Deed Document - Timely submission of the affidavit can positively impact the purchasing process.
Ucc 308 - The UCC 1-308 form ensures transparency by notifying all relevant parties of rights reserved.
Detailed Guide for Writing Ada Dental Claim
Filling out the ADA Dental Claim form is an essential step in ensuring that dental services are properly billed to your insurance provider. Completing the form accurately will help facilitate the claims process and ensure that you receive the benefits you are entitled to.
- Type of Transaction: Mark all applicable boxes for the type of transaction you are submitting, such as "Statement of Actual Services" or "Request for Predetermination/Preauthorization."
- Predetermination/Preauthorization Number: If applicable, enter the predetermination or preauthorization number.
- Policyholder/Subscriber Information: Fill in the policyholder's name, address, city, state, and zip code.
- Insurance Company/Dental Benefit Plan Information: Provide the company or plan name, address, city, state, and zip code of the insurance provider.
- Date of Birth: Enter the policyholder's date of birth in MM/DD/CCYY format.
- Gender: Indicate the policyholder's gender by marking "M" for male or "F" for female.
- Policyholder/Subscriber ID: Provide the policyholder's Social Security Number (SSN) or identification number.
- Other Coverage: If there is other dental or medical coverage, answer "Yes" and complete items 5-11. If not, skip to the patient information section.
- Patient Information: Fill in the patient's relationship to the policyholder, student status, date of birth, gender, and address.
- Record of Services Provided: For each procedure, enter the procedure date, area, tooth number(s), procedure code, description, and fee.
- Missing Teeth Information: Mark each missing tooth with an "X" and enter total fees for the services.
- Authorizations: Sign and date to authorize payment of benefits directly to the dentist.
- Treatment Information: Indicate if the treatment is for orthodontics, and if so, provide the date the appliance was placed and months of treatment.
- Billing Dentist or Dental Entity: If applicable, fill in the name, address, and contact information for the billing dentist or dental entity.
After completing the form, review all entries to ensure accuracy. Any errors or omissions can delay processing. Once satisfied, submit the claim form along with any required documentation to the appropriate insurance company or dental benefit plan.