Blank 3613 A Form
Key takeaways
- The 3613 A form is specifically designed for use by various types of healthcare facilities, including Skilled Nursing Facilities and Assisted Living Facilities.
- When filling out the form, ensure all sections are completed accurately to avoid delays in processing.
- The form must be faxed to the designated number, 1-877-438-5827, or mailed to the Texas Department of Aging and Disability Services.
- Confidentiality is crucial; the form contains sensitive information that should only be shared with authorized recipients.
- Clearly identify the incident category, such as abuse or neglect, to facilitate proper investigation.
- Include detailed information about the individuals involved, including their functional abilities and level of supervision.
- Document any witnesses and their statements, as this can be vital for the investigation.
- Be aware that the form requires a summary of the investigation findings, which should be thorough and objective.
- Finally, ensure that the report is signed and dated by the appropriate authority to validate the submission.
Common mistakes
Completing the 3613 A form is a critical process for various healthcare facilities, yet many individuals encounter challenges that can lead to significant mistakes. One common error is neglecting to provide complete contact information. The form requires detailed entries, including the provider's name, address, and telephone number. Omitting any of these details can result in delays in processing the report, as the authorities may struggle to reach the provider for follow-up questions or clarifications.
Another frequent mistake involves misidentifying the incident category. The form lists several categories such as abuse, neglect, and drug diversion. Selecting the wrong category not only misrepresents the nature of the incident but can also hinder the appropriate response from the relevant authorities. It is essential to carefully assess the situation before making this selection to ensure accuracy.
Additionally, individuals often fail to include the date and time of the incident. This oversight can create confusion regarding the timeline of events, making it difficult for investigators to understand the context. Providing precise information about when the incident occurred is crucial for a thorough investigation and for any subsequent actions that may need to be taken.
Another common error is related to the information about the individuals involved. When detailing the alleged victim(s) or aggressor(s), it is important to provide complete and accurate details, including their functional ability and level of supervision. Incomplete information can lead to misunderstandings and may compromise the investigation's integrity.
Moreover, some individuals mistakenly fail to document the history of combativeness or similar allegations. This information can be vital in understanding the context of the incident and assessing potential risks. If such history exists, it should be clearly noted on the form to assist investigators in their analysis.
In terms of witness statements, another mistake occurs when individuals do not attach the necessary documentation. If there are witnesses to the incident, their statements should be included, ideally signed and notarized. This omission can weaken the report's credibility and limit the investigation's effectiveness.
Furthermore, a lack of clarity in describing the allegation is a common pitfall. The narrative section should be detailed and specific, providing a clear picture of what transpired. Vague descriptions can lead to misinterpretations and may ultimately affect the outcome of the investigation.
Another issue arises when individuals do not indicate whether treatment was provided following the incident. This detail is important for understanding the immediate response and any ongoing care that may be necessary for the individuals involved. Failing to include this information can obscure the full scope of the incident's impact.
Lastly, many individuals overlook the importance of signing and dating the report. A signature is not merely a formality; it signifies that the information provided is accurate and complete to the best of the reporter's knowledge. Neglecting to include this can lead to questions about the report's authenticity and can complicate the review process.
Misconceptions
- Misconception 1: The 3613 A form is only for skilled nursing facilities.
- Misconception 2: The form must be mailed even if it is faxed.
- Misconception 3: Only serious incidents require a 3613 A report.
- Misconception 4: The form is not confidential.
- Misconception 5: Anyone can fill out the form without proper training.
- Misconception 6: The 3613 A form is only relevant for immediate incidents.
This form is actually intended for a variety of facilities, including nursing facilities, assisted living facilities, and adult day care centers. It serves a broader purpose than many realize.
In fact, if the report is faxed, it should not be mailed. This can save time and resources for both the sender and the recipient.
While serious incidents like abuse or neglect certainly warrant a report, the form is also used for other incidents, such as power failures or environmental hazards, which can impact resident safety.
On the contrary, the 3613 A form contains privileged and confidential information. Unauthorized disclosure of this information is strictly prohibited and can have legal consequences.
While the form may seem straightforward, it is crucial that individuals filling it out understand the specific requirements and implications of the information being reported. Proper training ensures accuracy and compliance.
This form also plays a role in documenting patterns over time. A single incident may not seem significant, but repeated issues can indicate larger systemic problems that need addressing.
Dos and Don'ts
When filling out the 3613 A form, attention to detail is crucial. Here are some important dos and don'ts to keep in mind:
- Do ensure all required fields are completed accurately.
- Do double-check the contact information for the provider and the recipient.
- Do keep a copy of the submitted form for your records.
- Do submit the form via fax or mail as instructed, but never do both.
- Don't leave any fields blank unless specified.
- Don't include unnecessary personal information that is not requested.
- Don't forget to sign and date the form before submission.
- Don't use the form for purposes outside of the specified facilities.
Other PDF Forms
Show Rabbits - Legal requirements may mandate the use of pedigree records for show entries.
How Old Do You Have to Be to Take a Ged Test - Include your date of testing if you know it to help locate your records more quickly.
Having a reliable Medical Power of Attorney form is crucial, as it ensures that your healthcare decisions are managed by someone you trust when you cannot advocate for yourself. For those looking to complete this process in California, resources such as California PDF Forms can simplify the task, allowing individuals to tailor their healthcare directives according to personal preferences and legal requirements.
Music Performance Contract - Details of the performance, including the band name and type of performance, must be specified.
Detailed Guide for Writing 3613 A
After completing the 3613 A form, you will need to submit it to the appropriate authorities. Make sure to follow the submission guidelines carefully, whether you choose to fax or mail the document. Ensure that all necessary information is filled out accurately to avoid delays in processing.
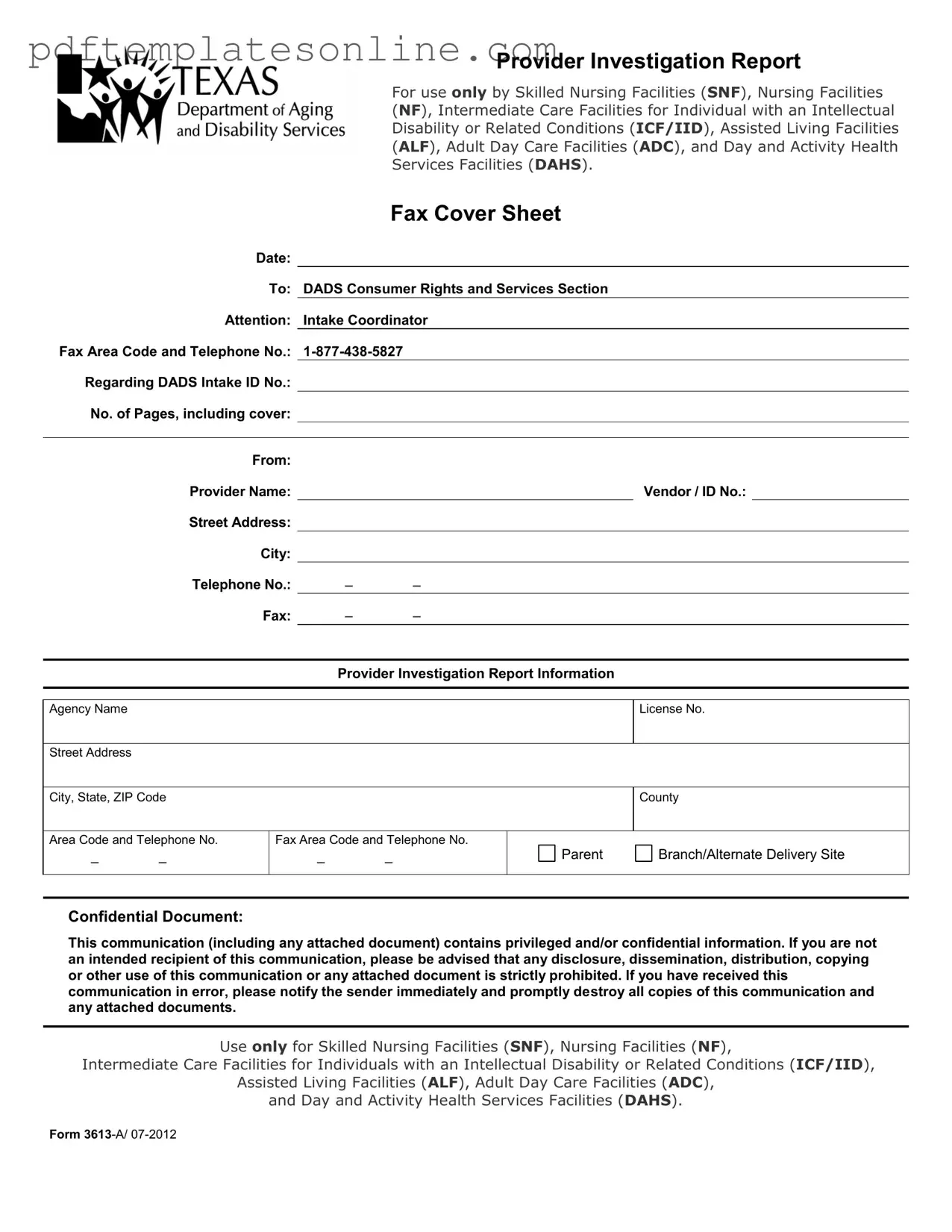
- Begin by filling out the Fax Cover Sheet at the top of the form. Include the date, recipient information, and your contact details.
- In the Provider Investigation Report Information section, enter the agency name, license number, street address, city, state, ZIP code, county, and contact numbers.
- Specify the Provider Type and include the vendor or ID number along with the provider's telephone and fax numbers.
- Identify the Incident Category by checking the appropriate box, such as Death, Abuse, Neglect, or others listed.
- Document who made the allegation and the date and time of the incident.
- Provide details about the Individual(s)/Resident(s) Involved. Include names, genders, social security numbers, dates of birth, functional abilities, and levels of supervision.
- For each individual, indicate if they are interviewable and their capacity to make informed decisions. Note any history of combativeness or similar allegations.
- Fill in the details for the Alleged Perpetrator(s), including their name, date of birth, social security number, and how they were identified.
- Check if the alleged perpetrator denied or confirmed the allegation and if there is a history of similar allegations.
- Note whether there were any witnesses to the incident and provide their names and contact information.
- Describe the allegation in detail and indicate if there was any injury or adverse effect.
- Document the assessment date and time, along with a description of the assessment and any treatment provided.
- Complete the Provider Response section, including your signature, printed name, title, and date.